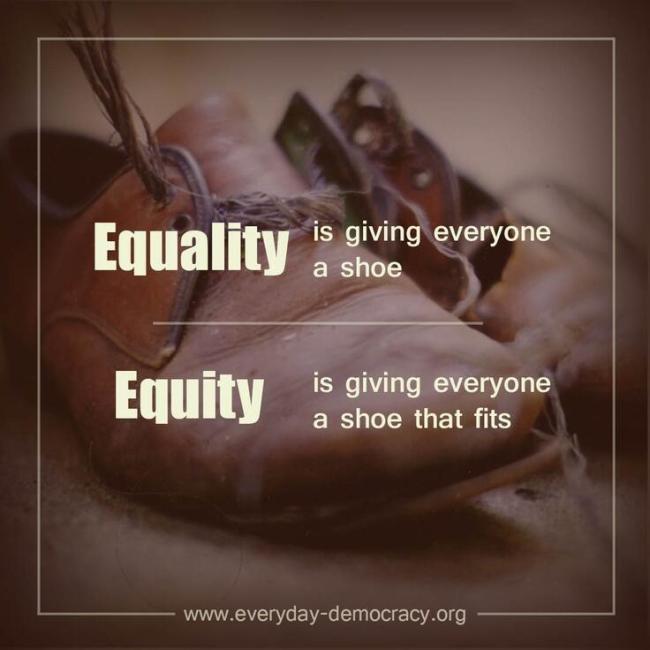
Social justice is defined as the fair distribution of laws that all people no matter their ethnic origin, gender, possessions, race, or religion are to be treated equally (Business Dictionary, n.d.). According to Braveman and Gruskin (2003) equity can be defined as social justice or fairness, based on the principles of fairly distributing resources in society. There is a difference between equity and equality. The image that is attached at the beginning on the blog can explain the difference between equity and equality. Equality is giving every body the exact same things no matter their social status, state of health, or resources. Equity is giving people what they need to have the same outcome as others. Not all shoe sizes fit all; equality is giving everybody the same shoe and shoe size, equity is giving everybody a good shoe that fits.
The current distribution of resources is unfair and consequently leads to inequality in the health among individuals. Everyone should have access to the ‘highest attainable standard of health”(Bravement & Gruskin, 2003), however, currently it only pertains to the wealthy. This is a social justice issue, the inequitable distribution of resources allow for a greater health in people with higher social status and income.
There is also inequity in the access and usability of information from technology. Britz (2004) describes the term ‘information poverty’ as a situation in which individuals and communities do not have the skills, abilities, or materials to have access to information, understand it and use it effectively. Technology has grown and has caused a change in the knowledge of certain populations; however, it has intensified the gap between the rich and the poor. Human decision making and problem solving is supported by reliable information. The ability to use information and apply it is determined by the level of skills, experience and education (Britz, 2004).
Individuals from a higher social status are more likely to attend prestigious schools and attain a better education than those with a lower social status (Doob, 2013) Therefore, people with higher education are at a greater advantage to access and interpret health information they are exposed to online. The distribution of resources is creating a greater advantage for people in the higher social classes.
Consequently, the inequity of distribution of resources puts lower class populations who are already at a disadvantage at an even further disadvantage, as they might not be able to access, interpret, or apply the health information.If there was health equity it would mean that there is no difference in the health of people of different social classes, race, gender, background as everyone would receive the resources they need to attain the highest standard of health possible (Bravement & Gruskin, 2003). Our society has to work towards equity in health information distribution from technology among all the social classes, and make sure that it is applicable and effective.
References
Doob, C. S. (2013). Understanding stratification, inequality, and social class in the u.s. Retrieved from https://www.boundless.com/sociology/understanding-stratification-inequality-and-social-class-in-the-u-s/
Britz, J. J. (2004). To know or not to know: A moral reflection on information poverty. Journal of Information Science, 30(3), 192-204. doi: 10.1177/0165551504044666
Braveman, P., & Gruskin, S. (2003). Defining equity in health. Journal of Epidemiology and Community Health, 57(4), 254–258. doi: 10.1136/jech.57.4.254
Queer, O. (Photographer). (2013, November 12). Equality vs Equity [Print Photo]. Retrieved from https://twitter.com/queerontario/status/403507508578226176/photo/1